Introduction
The microbiome
The microbiome is a diverse collection of bacteria, viruses, fungi, and other microorganisms living on our skin, in our mouths, nasal passages, and urogenital tracts . Each of these areas harbors a specialized microbial community finely tuned to its specific environment. Morover, they have the potential to impact our health, mood, and overall well-being in profound ways. In total the microbiome comprises approximately 38 trillion bacterial cells compared to our 30 trillion human cells. By this parameter, we are more microbial than human.
Our symbiotic relationship with the microbiome
Our symbiotic relationship with these microorganisms dates back millions of years, featuring ancient bacteria that have co-evolved alongside humans. The microbiome is as unique as a fingerprint. It varies from one person to another due to differences in genetics, what we eat, our lifestyle, and our environmental exposures. Microbial companionship begins at birth, influenced significantly by our mode of delivery and early diet. Moreover, it continues to develop throughout our lives in response to our food preferences, lifestyle, and age.
The Microbiome as a “New Organ”
The microbiome is regarded by some researchers as a “new organ” because of its critical functions. It plays a role in digestion, immune response, and even how our bodies metabolize medications. It also fulfills essential roles, from synthesizing vital vitamins, to helping our immune system learn to distinguish harmful invaders from harmless ones. Perhaps even more remarkably, certain microbes within our gut even produce neurotransmitters including serotonin and dopamine. This represents one component of the direct link between gastrointestinal health to our mental well-being through the gut-brain axis.
Revolutionizing Medicine and Health
Our understanding of these microscopic co-inhabitants offers a revolutionary approach to medicine and health, and represents a new realm of personalized medical treatments. For instance the microbiome contains at least 200 times more genes than the human genome. This indicates the immense capabilities encoded in this “second genome” and lays the groundwork for future research and therapeutic innovation.
The History and Discovery of the Microbiome
Early Insights

Portrait by Jan Verkolje via Wikimedia Commons
Our understanding the human microbiome began centuries ago. Antonie van Leeuwenhoek made the first observations of microorganisms in the late 17th century using a rudimentary microscope. Leeuwenhoek referred to these bacteria and other organisms as “animalcules.” His discoveries laid the groundwork for the field of microbiology. The significance of these microorganisms to human health and disease remained largely unexplored for many years, however.
In the 19th century, scientists like Louis Pasteur and Robert Koch established the germ theory of disease. They demonstrated that specific microbes cause specific diseases. This was a monumental leap in understanding infectious diseases. However, it inadvertently cast microbes in a predominantly negative light, overshadowing the potential beneficial roles of the body’s microbial inhabitants.
The Birth of Microbiome Research
The 20th century brought with it significant breakthroughs that paved the way for modern microbiome research. Researchers began to recognize that the body harbors a vast array of microbes that do not cause disease and might, in fact, play beneficial roles. One of the pivotal figures in this shift was Yoshimi Benno and his team at the Japan Collection of Microorganisms, who at the turn of the century, began cataloging the bacteria present in the human gut, revealing a complex ecosystem.

In the early 21st century, the Human Microbiome Project (HMP), launched by the National Institutes of Health in the United States, marked a significant milestone in microbiome research. The project aimed to identify and characterize the microorganisms found in association with both healthy and diseased human bodies. This initiative, alongside the MetaHIT project (Metagenomics of the Human Intestinal Tract) in Europe, provided unprecedented insights into the diversity and function of the human microbiome, highlighting its vital role in health and disease.
Understanding Its Importance
As research progressed, scientists began to uncover the microbiome’s complex relationship with the human body. One of the key figures in demonstrating the microbiome’s impact on health was Jeffrey Gordon and his team at Washington University in St. Louis. Their research in the early 2000s on the gut microbiome’s role in obesity and metabolism was groundbreaking, illustrating how the microbiome influences our physiology in profound and previously unimagined ways.
This body of research marked a significant shift in our understanding of microbes. No longer were they seen solely as agents of disease, but rather as essential partners in maintaining health. The concept of dysbiosis, or the imbalance of these microbial communities, is linked a number of health issues. These range from inflammatory bowel disease to diabetes and even mental health conditions. This has spurred research focused on harnessing the power of microbiome communities to promote health and prevent disease.
The distribution and development of the Human Microbiome
Diversity and Distribution
The human microbiome represents a complex and varied ecosystem, with each body region hosting specialized microbial communities. For instance, the gut microbiome, is primarily composed of the Bacteroidetes and Firmicutes phyla. These species are vital for food digestion and nutrient synthesis, as highlighted by Dr. Gordon.
On the other hand, the skin microbiome maintains an acidic environment and breaks down oils. It , features organisms such as Staphylococcus and Cutibacterium. Moreover, the oral microbiome includes bacteria like Streptococcus and Actinomyces, essential for oral hygiene and impacting systemic health.
These communities are dynamic, influenced by age, diet, lifestyle, and environmental factors. Dr. Peter Turnbaugh at the University of California, San Francisco, has shown how dietary choices, particularly fiber-rich diets, can significantly alter the gut microbiome’s composition, promoting diversity and robustness.
Formation and Development
The microbiome’s development begins at birth, with the mode of delivery impacting the newborn’s initial microbial exposure. Dr. Maria Gloria Dominguez-Bello at Rutgers University has demonstrated how vaginal deliveries expose infants to maternal vaginal and fecal microbes, whereas cesarean sections result in a microbiome initially dominated by skin-associated and environmental microbes. Moreover, breastfeeding, introduces beneficial bacteria and prebiotic compounds, important for early microbiome development.
As individuals age, their microbiome evolves. It diversifies with the introduction of solid foods and later shifting during adolescence, adulthood, and old age due to diet, lifestyle, health status, and medication use. Dr. Rob Knight at the University of California, San Diego, has noted that microbiome diversity tends to decrease with age, influencing health and disease susceptibility.
Understanding the microbiome’s variation across body locations and its evolution over a lifetime is key to developing precise interventions for maintaining or restoring healthy microbial balance. This insight lays the groundwork for personalized medicine. Treatments can be customized to an individual’s unique microbiome profile, opening new paths for disease prevention and therapy.
The Microbiome in Health and Disease
Digestive Health and the Microbiome
The Microbiome’s Role in Digestion

The microbiome plays a pivotal role in digestive health. It aids in the breakdown of dietary fibers, nutrient absorption, and the synthesis of essential vitamins, thereby enhancing the host’s overall well-being. Moreover, the gut microbiota breaks down complex carbohydrates and fibers—substances resistant to digestion by human enzymes—into short-chain fatty acids (SCFAs) such as butyrate, propionate, and acetate. These SCFAs are important for maintaining gut barrier integrity, regulating metabolism, and providing energy for colonic cells .
Vitamin Synthesis by Gut Bacteria
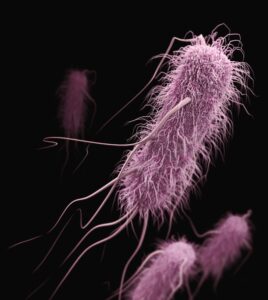
Additionally, certain gut bacteria are essential for synthesizing critical vitamins, enhancing our nutritional well-being. For instance, bacteria like Escherichia coli and various species of the genera Bacteroides and Fusobacterium produce vitamin K. This molecule is vital for blood clotting and bone health.
Similarly, B vitamins, necessary for metabolic processes and energy production, are synthesized by specific gut microbes. Bifidobacterium and Lactobacillus species contribute to the production of biotin (B7) and folate (B9). Vitamin B12, essential for brain function and blood formation, is produced by certain Propionibacterium species.
Impact on Digestive Health Conditions
From CDC via Unsplash
The composition and function of the gut microbiota links to various digestive health conditions. This includes inflammatory bowel disease (IBD). In individuals with IBD, significant alterations in the gut microbiome have been observed. These are characterized by decreased microbial diversity and a shift in the balance of beneficial versus harmful bacteria. These changes can exacerbate the inflammatory responses in the gut, contributing to the disease’s pathogenesis.
Studies have shown that certain bacteria, such as those from the Firmicutes and Bacteroidetes phyla, are involved in maintaining gut health and modulating inflammation. Conversely, a reduction in these beneficial microbes and an increase in pathogenic ones like Escherichia coli and Enterococcus faecalis often associates with IBD flare-ups. These insights into the microbiome’s role in digestive disorders underscore the potential of therapeutic strategies such as probiotics, prebiotics, and dietary modifications to restore microbial balance and alleviate symptoms.
Immune System Modulation: The Microbiome’s Role in Immune Function
The Microbiome as an Immune System Educator
The human microbiome plays a critical and complex role in modulating the immune system, serving as an essential mediator between the body and its environment. This interplay is pivotal for maintaining health and protecting against diseases. The gut microbiome, in particular, is a central player in the development, education, and function of the immune system.
The microbiome is instrumental in educating the immune system from an early age. It teaches the immune system to differentiate between harmful pathogens that need to be attacked, and commensal microbes that should be tolerated. This process is important for developing a balanced immune response, capable of effectively combating infections while avoiding overreactions that can lead to allergies and autoimmune conditions. For instance, certain gut bacteria promote the production of regulatory T cells. This response helps prevent autoimmune reactions by suppressing inflammatory reactions.
Defense Against Pathogens
The microbiome provides a critical line of defense against pathogenic invaders. This occurs through mechanisms such as competitive exclusion, where beneficial microbes outcompete pathogens for nutrients and space, and the production of antimicrobial substances. Additionally, the microbiome can enhance the barrier function of the gut lining, making it more difficult for pathogens to penetrate and cause infections. Collectively, these activities of the microbiome help to prevent the colonization and spread of harmful organisms.
Modulating Inflammatory Responses
Chronic inflammation is a hallmark of many immune-mediated diseases, and the microbiome plays a significant role in modulating inflammatory responses. An imbalance in the microbiome, or dysbiosis, can lead to heightened inflammation. This contributes to the development of conditions such as inflammatory bowel disease (IBD), rheumatoid arthritis, and even certain cancers. Conversely, a healthy and diverse microbiome can help regulate the immune system’s inflammatory pathways, reducing the risk of chronic inflammation and associated diseases.
Impact on Vaccine Efficacy
Recent research has also highlighted the microbiome’s influence on the efficacy of vaccines. The composition and diversity of an individual’s microbiome can affect how the immune system responds to vaccination, potentially impacting the vaccine’s effectiveness. This area of study underscores the microbiome’s broad role in immune function and its potential implications for public health interventions.
Gut-brain Axis: Influence of Gut Microbiota on Mental and Neurological Health
The gut-brain axis is a bidirectional communication system connecting the gastrointestinal tract and the central nervous system, significantly impacting mental and neurological health. Gut bacteria synthesize key neurotransmitters like serotonin, dopamine, and GABA. Imbalances in gut microbiota can disrupt neurotransmitter levels, leading to mood disorders such as depression and anxiety.
Furthermore, the gut microbiota influences brain health by modulating the immune system and the body’s stress response. As previously noted, an imbalanced microbiome can cause chronic inflammation. This is associated with psychiatric and neurodegenerative diseases. It can also lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, affecting stress reactivity and behavior.
Research also links the gut microbiota to neurodevelopmental disorders like autism spectrum disorder (ASD), with gut microbiome variations potentially affecting ASD symptoms. Similarly, dysbiosis is implicated in neurodegenerative diseases such as Alzheimer’s and Parkinson’s, through inflammation and altered neurotransmitter levels. Targeting the gut microbiome offers promising therapeutic avenues for managing these conditions. Moreover, these effects on mental and neurological health underscore the critical role of maintaining a healthy gut-brain connection.
Metabolic Health: Relationship between the Microbiome and Metabolism
The makeup of the gut microbiome significantly impacts nutrient metabolism, energy balance, and insulin sensitivity. This suggests that targeting the gut microbiome could offer revolutionary strategies for the management of metabolic health issues. For instance, gut microbes break down dietary fibers into short-chain fatty acids like acetate, propionate, and butyrate, influencing glucose regulation, lipid metabolism, and appetite control. These microbial activities can affect energy extraction from food, potentially leading to increased calorie intake and fat storage, thereby influencing obesity risk.
Moreover, dysbiosis, or imbalance in the gut microbiome, links to insulin resistance. This suggests that modulating the gut microbiota could offer new approaches for type 2 diabetes therapy.
Additionally, the microbiome’s influence on systemic inflammation is a key factor in metabolic syndrome. This suggests that microbiome-targeted interventions that mitigate inflammation could be used to prevent or treat metabolic disorders.
Skin Health: Influence of Skin Microbiota on Dermatological Conditions
The skin microbiota, comprises bacteria, fungi, viruses, and mites. It is essential for skin health, defending against pathogens, modulating immune responses, and maintaining the skin’s integrity. However, it also links to skin conditions like acne, eczema, psoriasis, and rosacea. This make it a focus for microbiome-targeted dermatological therapies.
Dysbiosis, or microbial imbalance, can exacerbate these conditions by causing inflammation, immune reactions, and barrier disruption. For instance, excess Propionibacterium acnes contributes to acne, while microbial imbalances are noted in eczema and psoriasis.
However, emerging evidence suggests that adjusting the skin microbiota can improve eczema and psoriasis by modulating inflammatory responses and skin barrier functions. This may indicate that dermatological interventions like topical probiotics and prebiotics can treat these conditions by restoring microbial equilibrium, reducing inflammation, and enhancing skin health.
Microbiome disbiosis and chronic disease
Dysbiosis, a term for the imbalance in the microbiome, increasingly links to a variety of chronic diseases. This underscores the crucial role that these microbial communities play in maintaining health. In addition to IBD, dysbiosis associates with obesity, diabetes, and certain cancers. Once again, a reduction in microbial diversity or an over representation of certain harmful bacteria can lead to inflammation. This is a common pathway in the development of these conditions.
As we discussed earlier, specific changes in the gut microbiota composition associate IDB. Similarly, obesity and diabetes link to alterations in the gut microbiome that affect metabolic functions and inflammation. Moreover, emerging research suggests that the microbiome may influence the risk of developing certain types of cancer, such as colorectal cancer. This may occur through the production of carcinogenic compounds or the modulation of inflammation.
Antibiotic treatments and pathogenic infection
The microbiome plays a defensive role in protecting against infections by competing with pathogens for nutrients and space, producing antimicrobial compounds, and modulating the host’s immune response. However, the use of antibiotics can have a significant impact on microbial diversity by killing off beneficial bacteria along with harmful ones. This disruption can lead to an increased risk of infections, such as those caused by Clostridioides difficile, a pathogen that can proliferate in the gut following antibiotic treatment.
Moreover, the misuse and overuse of antibiotics has contributed to the rise of antibiotic-resistant bacteria, posing a significant challenge to public health. Antibiotic exposure can also lead to a loss of microbial diversity. This can diminish the microbiome’s resilience, making it more difficult to recover from disturbances and resist colonization by pathogens.
Microbiome-Based Disease Treatments
Microbiome Therapeutics
The rapidly advancing field of microbiome research has dramatically changed our understanding of human health and disease. Moreover, it is introducing innovative therapeutic strategies for a wide range of conditions. These microbiome-based treatments leverage the complex relationship between the human microbiome and various health states. It represents a significant shift from traditional pharmaceutical methods to more personalized and holistic approaches.
Fecal Microbiota Transplantation (FMT)
FMT has emerged as a groundbreaking treatment, especially for Clostridioides difficile infections, demonstrating the microbiome’s key role in digestive health. Its success has led to further exploration of its potential for treating inflammatory bowel diseases and metabolic syndromes.
Probiotics and Prebiotics in Treatment
Probiotic and prebiotic therapies have broadened the possibilities for microbiome manipulation, offering targeted ways to restore or maintain a healthy microbial balance. These interventions are proving beneficial not only for gut health but also for influencing immune, mental, and metabolic diseases. In the realm of immune health, the potential of probiotics and prebiotics to modulate systemic inflammation and immune responses opens new pathways for managing conditions such as Rheumatoid Arthritis and Multiple Sclerosis.
Mental Health and Psychobiotics
In mental health, psychobiotics represent a new therapeutic direction for managing disorders such as depression, anxiety, and Autism Spectrum Disorder). These approaches, targeting the gut-brain axis, underscore the significant impact of the gut microbiota on mental well-being.
Addressing Metabolic Diseases
Research into the microbiome’s role in metabolic diseases like obesity, T2D, and Non-alcoholic Fatty Liver Disease is expanding. Personalized nutrition and microbiome-targeted therapies such as probiotics and FMT are being explored for their potential to enhance metabolic health. This underscores the microbiome’s critical function in regulating energy balance and metabolism.
Everyday Impacts and Lifestyle Considerations
Our daily choices, including our diet and lifestyle, significantly influence our microbiome. Recognizing how these factors interact with the microbiome helps establish habits that promote a balanced and healthy microbial community.
Diet and the Microbiome

Diet significantly affects the gut microbiome’s composition and function. Consuming dietary fiber found in fruits, vegetables, and whole grains can foster a diverse and healthy microbiome. These high-fiber foods act as prebiotics, nourishing beneficial gut bacteria and encouraging their proliferation. Conversely, a diet rich in processed foods and sugars may diminish microbial diversity and lead to dysbiosis, potentially causing health complications.
Probiotics and Prebiotics
Incorporating probiotics and prebiotics into the diet is a proactive strategy to positively impact the gut microbiome. Consuming foods rich in probiotics, such as yogurt, kefir, and fermented vegetables, introduces beneficial bacteria to the gut, supporting health and well-being. Prebiotics, indigestible dietary fibers, feed these beneficial bacteria, promoting their growth and contributing to gut health and disease prevention.
Hygiene Practices
Modern hygiene practices play a crucial role in preventing infectious diseases. However it also may have negative effects on microbial diversity. Excessive cleanliness and the widespread use of antibacterial products may contribute to a decrease in microbial diversity. This can lead to an increase in autoimmune and allergic conditions. A balanced approach to hygiene that includes exposure to a diverse array of microbes, is essential for developing a strong immune system and a healthy microbiome. Adopting sensible hygiene practices without overusing antibacterial products and engaging with natural environments can help maintain microbial diversity.
Latest Research and Innovations in Microbiome Science
Advanced Therapeutic Modalities
FMT is broadening its application scope, moving beyond Clostridioides difficile infection treatment to address neurological conditions, including Autism, multiple sclerosis and Parkinson’s (Vendrik, et al. 2020). Moreover, promising results have also been exhibited in patients with various autoimmune diseases following FMT (Seida et al. 2024). The concept utilizing the microbiome in personalized care is also gaining traction. Researchers are exploring how information stored within microbiomes may be used in early detection and prognostic assessment of disease in at-risk populations. Conversely, treatment aimed at modulating the microbiome may be tailored to the individual (Ratiner, 2023).
In the realm of engineered probiotics, researchers are utilizing synthetic biology to develop probiotics that can target metabolic and infectious diseases, as well as immune diseases, allergies as well as cancers (Chua et al. 2017). Remarkably, researchers are developing novel approaches for genetically engineering unculturable microbes directly within the gut microbiome (Careaga 2024).
Dietary Interventions and Personalized Nutrition
Dr. Erica Sonnenburg and Dr. Justin Sonnenburg at Stanford University have contributed significantly to our understanding of how diet influences the microbiome, advocating for high-fiber diets to promote microbial diversity (Sonnenburg & Sonnenburg, 2019). Personalized nutrition is being advanced researchers exploring how individual microbiome analyses can inform personalized dietary recommendations (Liu et al. 2020).
Technological Innovations and Diagnostics
Researchers are developing methods for using AI to analyze microbiome microbiome genetic data (Zeng et al. 2021). Wearable and ingestible sensor technologies are being developed by Dr. Giovanni Traverso at MIT, offering new ways to monitor gut health in real-time as reported in MIT News.
Hygiene Hypothesis and Microbial Diversity
Reevaluating hygiene practices in light of microbial diversity, Dr. Martin Blaser at Rutgers University has highlighted how modern hygiene practices might be contributing to decreased microbial diversity and the rise in non-communicable disease in the 20th and 21st centuries. Dr. Maria Gloria Dominguez-Bello at New York University is studying the impact of environmental microbiomes on human health, suggesting ways to prevent the loss of microbial diversity in urban environments (Dominguez-Bello et al., 2018).
Microbiome Test Kits?
Microbiome test kits are consumer-friendly packages that allow individuals to collect samples (usually fecal samples) at home, which are then sent to a laboratory for analysis. The primary focus of most kits is the gut microbiome, although some kits are designed for analyzing the skin, oral, or vaginal microbiomes.
These kits aim to identify the various bacteria, fungi, and other microorganisms present and provide an analysis of the microbial diversity and composition. Users may receive recommendations for dietary or lifestyle changes aimed at improving their microbiome health, potentially leading to better overall health, digestion, and even mental well-being.
However, it’s important to approach these kits with a critical mindset. Certain microbial profiles have been observed to associate with particular health conditions. The science of the microbiome is still in its infancy, however. However, direct causation, and the implications for disease prevention or treatment are not yet fully understood.
Ongoing Challenges
Despite the remarkable strides in microbiome research and its potential applications, the field faces several ongoing challenges. A primary concern is the complexity of the microbiome itself. The vast diversity of microbial species and their interactions within the human body makes it difficult to pinpoint specific causal relationships between microbiota and health outcomes.
In addition, there’s a pressing need for standardized methodologies in microbiome research to ensure reproducibility and comparability across studies. As the field advances, addressing these challenges will be crucial for realizing the full therapeutic and diagnostic potential of microbiome science.
Moreover, translating findings from controlled laboratory studies to effective, safe treatments in humans involves navigating a labyrinth of logistical and regulatory hurdles. Additionally, ethical considerations, particularly regarding data privacy, and the implications of manipulating the human microbiome, add another layer of complexity.
Conclusion
Exploring the human microbiome opens up new pathways for understanding how the myriad microorganisms living within and on us influence our and diseases are influenced by. This area of research, burgeoning with potential, is reshaping the future of healthcare, offering innovative solutions tailored to individual needs. The impact of these microbial communities on mental well-being, immune responses, and metabolic processes underscores the possibility of a healthcare revolution grounded in personalized medicine.
Looking ahead, the scope for microbiome research in transforming medical practices is immense. Advances in this field promise to introduce treatments and therapies that leverage our microbial counterparts for disease prevention and management. With technological progress and deeper insights into microbial interactions, we are edging closer to unlocking new therapeutic avenues that could alter our approach to healthcare significantly.
Navigating this promising future requires addressing the challenges of ethical considerations in microbiome manipulation and the rigorous translation of research findings into effective clinical applications. Collaboration across scientific, clinical, and regulatory communities will be crucial to harness the full potential of microbiome research while ensuring safety and efficacy.
In essence, the study of the human microbiome highlights a shift towards healthcare that is personalized, effective, and informed by a profound understanding of the microorganisms that share our bodies. The exciting advancements in microbiome research point towards a new era of medical innovation, promising a future where health and disease management are fundamentally transformed.
References and Further Reading
Primary research and reviews
- The Integrative HMP (iHMP) Research Network Consortium. The Integrative Human Microbiome Project. Nature 569, 641–648 (2019). The Integrative Human Microbiome Project, comprised studies of dynamic changes in the microbiome and host under three conditions: pregnancy and preterm birth; inflammatory bowel diseases; and stressors that affect individuals with prediabetes.
- Gilbert, J.A., Blaser, M.J., Caporaso, J.G., Jansson, J.K., Lynch, S.V., & Knight, R. Current understanding of the human microbiome. Nature Medicine, 24, 392-400 (2018). A review of the latest insights into the human microbiome, highlighting its role in health and disease and the potential for microbiome-based therapies.
- Fishbein, Skye RS, Bejan Mahmud, and Gautam Dantas. Antibiotic perturbations to the gut microbiome Nature Reviews Microbiology 21.12: 772-788 (2023). This paper shows that antibiotic use disrupts the gut microbiome, potentially leading to various diseases, and highlights how emerging multi-omic techniques are uncovering factors that influence microbiome changes and recovery post-antibiotic treatment, aiding in developing strategies to minimize or reverse these effects.
- Graham, D. B., & Xavier, R. J. (2023). Conditioning of the immune system by the microbiome. Trends in Immunology. The microbiome influences the immune functions of mammals in various ways. The idea of conditioned immunity offers a model to understand these complex molecular mechanisms.
- Foster, J.A., Rinaman, L., & Cryan, J.F. (2017). Stress & the gut-brain axis: Regulation by the microbiome. Neurobiology of Stress, 7, 124-136. This article explores the intricate relationship between the gut microbiome and the brain, emphasizing the impact of microbial communities on mental health.
- Sampson, T.R., & Mazmanian, S.K. (2015). Control of brain development, function, and behavior by the microbiome. Cell Host & Microbe, 17(5), 565-576. This research article discusses the significant influence of the gut microbiome on brain development and function, shedding light on the gut-brain axis.
Books
These books offer a blend of scientific insight, practical advice, and compelling storytelling that can appeal to both experts in the field and general readers interested in health and science.
- “I Contain Multitudes: The Microbes Within Us and a Grander View of Life” by Ed Yong,
Ecco 2016. This book provides a captivating exploration of the microbial world and its profound impact on the lives of all organisms, including humans. Ed Yong masterfully explains complex scientific concepts in an accessible and engaging manner. - “The Microbiome Solution: A Radical New Way to Heal Your Body from the Inside Out” by Robynne Chutkan, Avery 2016. Dr. Chutkan offers practical advice on restoring and maintaining a healthy microbiome. This book combines scientific research with actionable recommendations for lifestyle changes that support gut health.
- “Gut: The Inside Story of Our Body’s Most Underrated Organ” by Giulia Enders,
Greystone Books 2015. With humor and scientific rigor, Enders takes readers on a journey through the human digestive system, highlighting the crucial role of the gut and its microbial inhabitants in overall health. - “Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues” by Martin J. Blaser, Henry Holt and Co. 2014. This book discusses the vital balance of the human microbiome and how modern medical practices, particularly the overuse of antibiotics, are disrupting this balance, leading to an increase in chronic diseases.
- “The Mind-Gut-Immune Connection: Understanding How Food Impacts Our Mind, Our Microbiome, and Our Immunity” by Emeran Mayer, Harper Paperbacks 2023. Dr. Mayer’s research illuminates how the essential dialogue between the myriad of microbes in our gastrointestinal tract and our body’s systems plays a pivotal role in our health, with disruptions in this interaction often leading to serious illness.
Blogs/Websites
- The Microsetta Initiative is a research project based out of UC San Diego with the goal to create a comprehensive map of the human microbiome that researchers, clinicians, school groups, or anyone can use to explore and research the human microbiome! You can help build the biggest, open-source human microbiome resource by contributing a microbiome sample and completing a food frequency questionnaire
- Gut Microbiota for Health Sponsored by the European Society for Neurogastroenterology & Motility (ESNM), this blog offers the latest news, research updates, and expert opinions on gut microbiota.
- Microbiome Digest – Bik’s Picks Curated by Dr. Elisabeth Bik, Microbiome Digest compiles the latest scientific research on microbiomes across different environments, including the human body.
Documentaries
- Hack Your Health: The Secrets of Your Gut (2024) Delve into the digestive system with this lighthearted and informative documentary that demystifies the role gut health plays in our overall well-being.
- The invisible extinction (2022) Marty Blaser and Gloria Dominguez-Bello, both partners in life and research, highlight how antibiotics and elective C-sections diminish our body’s beneficial bacteria, contributing to increased rates of obesity, diabetes, asta, and food allergies. They are dedicated to preserving and replenishing our vital microbes to combat these trends.
- Microbiota: The Amazing Powers of the Gut (2019) Within our gut, 100,000 billion bacteria like Fecalibacterium and Akkermansia muciniphila produce health-essential molecules. Though microscopic and complexly named, they have the potential to revolutionize medicine, unless modern lifestyle threats prevail.
- The Gut: Our Second Brain (2014) Our gut, home to 100,000 billion bacteria, acts as a “second brain” influencing our personalities and potentially affecting conditions like Parkinson’s through intestinal neuron degeneration.